For nurse practitioners in South Carolina, navigating the regulatory landscape is a crucial part of establishing and maintaining a successful practice. The Palmetto State recognizes the vital role NPs play in delivering high-quality healthcare, especially in underserved areas, but also sets specific guidelines to ensure patient safety and effective collaboration within the healthcare system. Understanding these guidelines isn’t just about compliance; it’s about building a robust and professional foundation for your career.
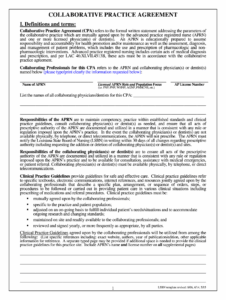
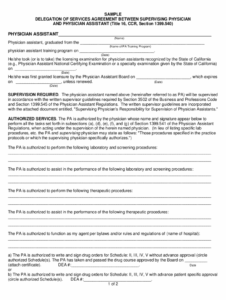
One of the cornerstone requirements for many nurse practitioners in South Carolina involves establishing a collaborative agreement with a physician. This document isn’t just a formality; it’s a detailed blueprint that outlines the professional relationship, scope of practice, and communication protocols between the NP and the collaborating physician. When looking to understand this requirement better, a well-structured south carolina nurse practitioner collaborative agreement template can serve as an invaluable starting point, offering clarity on the essential elements that need to be addressed.
The essence of a collaborative agreement is to foster a supportive environment where NPs can utilize their advanced training and skills while ensuring access to physician consultation and referral when necessary. It’s designed to formalize the lines of communication and define the parameters of the NP’s practice, ultimately benefiting patient care through a team-based approach. Without a properly executed agreement, an NP’s ability to practice fully and legally within the state may be significantly limited.
Understanding the Collaborative Agreement in South Carolina
A collaborative practice agreement in South Carolina is a legal document that outlines the relationship between a nurse practitioner and a supervising or collaborating physician. It’s designed to ensure that NPs have appropriate physician support and oversight, particularly concerning diagnosis, treatment, and prescriptive authority, while still allowing them to practice within their advanced scope. This agreement doesn’t mean the physician must be physically present at all times, but rather establishes a formal pathway for consultation and shared responsibility in patient care.
The necessity for such an agreement stems directly from South Carolina’s statutes and regulations governing advanced practice registered nurses (APRNs), including nurse practitioners. These laws specify that an NP’s practice must be conducted in accordance with a written collaborative agreement that details the roles, responsibilities, and areas of practice for both parties. It’s a mechanism to maintain accountability and ensure that patient care meets established standards, particularly when an NP is operating with a degree of independence.
Developing this agreement requires careful thought and clear communication between the NP and the collaborating physician. It’s more than just a signature; it’s a mutual understanding of how patient care will be delivered and how professional collaboration will function on a day-to-day basis. The goal is to create a document that is comprehensive, clear, and reflective of the actual practice environment and the specific needs of the patient population being served.
Essential Elements to Include
When drafting or reviewing a collaborative agreement, several key components must be addressed to ensure it meets state requirements and serves its intended purpose effectively. Neglecting any of these crucial elements could lead to compliance issues or operational misunderstandings.
-
Identification of Parties: Clearly state the full names, addresses, and license numbers of both the nurse practitioner and the collaborating physician. This establishes who is involved in the agreement.
-
Scope of Practice: Define the specific services and procedures the NP is authorized to perform, consistent with their education, training, and the South Carolina Nurse Practice Act. This might include diagnosing, treating, ordering and interpreting diagnostic tests, and managing patient care plans.
-
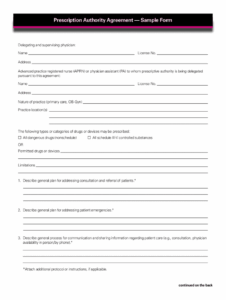
Prescriptive Authority: Detail the categories and types of medications the NP is authorized to prescribe, including any limitations or protocols for controlled substances, as dictated by state law.
-
Consultation and Referral Protocols: Outline the specific circumstances under which the NP must consult with the collaborating physician, as well as the procedures for patient referral to the physician or other specialists. This ensures appropriate oversight and access to specialized care.
-
Communication and Review Procedures: Describe how and when the NP and physician will communicate regarding patient care, review charts, and discuss practice issues. This often includes a defined schedule for regular meetings or chart reviews.
-
Termination Clause: Include provisions for how the agreement can be terminated by either party, including required notice periods, to ensure a smooth transition of patient care.
Moreover, the agreement should specify the geographic locations where the NP will practice under the agreement and acknowledge the respective responsibilities for professional liability and malpractice insurance. Ensuring all these details are clearly articulated will provide a solid framework for effective collaboration.
Navigating the Process and Finding Resources
The process of establishing a collaborative agreement involves more than just drafting a document; it requires finding the right collaborating physician, fostering a professional relationship built on trust, and ensuring the agreement complies with all state regulations. For many new NPs, identifying a physician willing to enter into such an agreement can be one of the initial challenges, often requiring networking within professional circles and healthcare organizations.
Once a potential collaborator is identified, both parties must engage in open dialogue to define the terms of their professional relationship, aligning expectations regarding patient care, communication frequency, and areas of responsibility. It’s wise for both the NP and the physician to seek independent legal counsel to review the proposed agreement, ensuring it protects their individual interests and adheres to all South Carolina laws and regulations. This legal review can help identify any potential ambiguities or omissions before the agreement is finalized.
Resources for guidance can be found through the South Carolina Board of Nursing, which often provides guidelines or FAQs regarding collaborative practice agreements. Professional organizations for nurse practitioners in South Carolina are also excellent sources for information, networking opportunities, and sometimes even sample language for agreements. While a comprehensive south carolina nurse practitioner collaborative agreement template can provide an excellent starting point, remember that each agreement should be tailored to the specific practice setting and the unique professional relationship between the NP and the collaborating physician.
A well-crafted collaborative agreement is more than a legal necessity; it’s a foundational document that empowers nurse practitioners to deliver comprehensive, high-quality care to their patients within the robust framework of South Carolina’s healthcare system. It solidifies the professional partnership, ensuring that both the NP and the collaborating physician are clear on their roles and responsibilities, which ultimately translates to better patient outcomes and a more harmonious practice environment.
Approaching the collaborative agreement with diligence and attention to detail is a testament to an NP’s commitment to professional excellence and patient safety. By carefully defining the parameters of practice and establishing clear communication channels, nurse practitioners can thrive in South Carolina, contributing significantly to the health and well-being of the communities they serve.